*Photo by Nadezhda Moryak from Pexels
What is PCOS?
PCOS is a leading cause of infertility, impacting as many as 5 million women of childbearing age in the US, however, the condition often causes challenges well beyond childbearing years. While the exact cause of PCOS is not yet known, it is thought to be multifactorial with an underlying genetic component. Typically women with PCOS suffer from insulin resistance. The cells of the body do not respond appropriately to insulin, requiring an increased insulin release to properly manage blood sugars. In turn, women with PCOS are at higher risk for type 2 diabetes. They also produce higher levels of androgens, such as testosterone, which contributes to the majority of PCOS symptoms.
Typically women with PCOS have an inappropriate ratio of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This negatively impacts follicle development, and thus egg growth. This poor egg development results in either dysfunctional ovulation, or anovulation (or lack of ovulation).
Symptoms associated with PCOS
PCOS can present in a variety of ways, and by definition is diagnosed based on a multifactorial presentation. Symptoms of PCOS typically result due to elevated insulin and androgen production. Some common symptoms of PCOS include:
- Acne
- Overgrowth of facial and body hair
- Anovulation (Absent ovulation)
- Irregular or prolonged cycles
- Polycystic ovaries, with “string of pearls” appearance on ultrasound
- Weight gain
- Difficulty losing weight
- Hair loss
- Infertility
The PCOS Diagnosis
Unfortunately, there is no single test that can determine if a person has PCOS. Instead, the clinical diagnosis is made if a woman has at least 2 of the following:
- Ovarian dysfunction, such as cycle irregularity or absent periods due to anovulation
- Elevated androgens (male hormones)
- Polycystic and enlarged ovaries as seen on ultrasound
It is important to note that a single presentation of one of these symptoms is not enough to diagnose PCOS. Since other conditions can cause ovulation disorders, such as thyroid dysfunction, it is important to consult your physician if you suspect you have an ovulation problem.
PCOS and Fertility
Believe it or not, PCOS is the most common disorder of ovulation in women of childbearing age. In order for conception to be possible, the ovary must mature and release an egg. In PCOS the egg may not mature as it should. Secondly, while the egg may mature, the follicle may not rupture as it should. For women with PCOS who do ovulate without the assistance of medication, conception is possible, but predicting when ovulation will occur can be challenging particularly if cycles are highly irregular.
Supporting Fertility in PCOS: A Conventional Approach
Typically, PCOS treatment addresses the concerns a woman may have based on her symptoms and goals, such as infertility, weight gain, excess hair growth, and acne.
Women with PCOS who want to address fertility are often prescribed medications to support ovulation, such as Letrozole and Clomid. Since PCOS typically includes ovulatory challenges, inducing ovulation with medications can restore fertility in some women with PCOS.
Metformin is used to increase insulin sensitivity, which in turn can help lower androgens. Some women with PCOS notice improved cycle regularity and ovulation with metformin but the results are inconsistent. In addition, some women are prescribed Metformin in combination with other medications, such as Clomid and Letrozole.
For those who wish to establish a regular cycle and are not trying to conceive, many doctors prescribe hormonal birth control. Many symptoms of PCOS improve while on birth control, as androgen production is lowered, however, symptoms return upon discontinuation.
Using Lifestyle and Diet to Support Hormone Health
PCOS is a hot topic in the lifestyle and natural health world. Recommendations vary widely between specialists in this area. If you have PCOS, you likely have heard (perhaps unwanted) advice that might directly contradict what you have read or heard. Despite this, there are some main ideas that most specialists agree upon.
- Exercise: Exercise can help reduce insulin resistance, which is paramount in PCOS. Beyond the systemic health benefits of exercise, it can also help lower insulin and androgen production and contribute to weight loss.
- Lower glycemic foods: Diet again is a very controversial topic in the PCOS world. While some recommend the keto diet, others recommend a whole food plant-based diet, and everything in between. Confused? Me, too. However, since high glycemic foods require more insulin to maintain normal glucose levels, and because women with PCOS generally struggle with insulin resistance requiring an even higher production of insulin, choosing foods which are lower on the glycemic index is generally recommended to prevent excessive insulin release.
- Support: Managing PCOS can be very challenging and isolating, especially when trying to conceive. If you have PCOS, you are not alone, and chances are you know someone else who struggles with PCOS, as well. Whether you find support virtually or in-person, recognize that you deserve a shoulder to lean on when the journey is stressful and there are many support groups and counseling services available.
- Supplementation: Several PCOS specialists recommend supplementation. Since this is a very individualistic need, please speak to your doctor before beginning any supplement regimen.
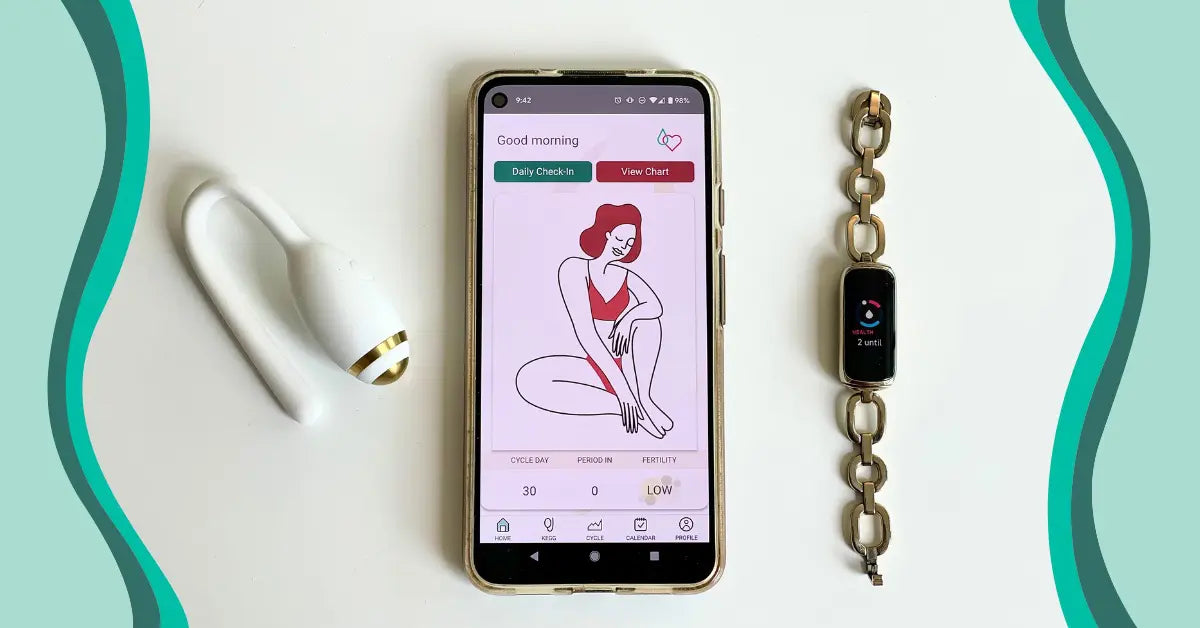
PCOS and kegg
While kegg is not clinically tested in women with PCOS, many women with PCOS who ovulate and have periods have been able to identify their fertile window thanks to kegg.
LH testing is of limited benefit to many women with PCOS as LH levels often remain elevated throughout the cycle or may surge multiple times during the cycle.
With kegg, women with PCOS who ovulate are able to look at their trend line data to discern when they have entered their fertile window. Since the electrolytes in the cervical fluid fluctuate according to the hormonal changes of the cycle, the kegg user can look for descending values on their kegg readings to predict when they are entering their fertile window. While kegg does not detect ovulation, the rise that occurs at the end of the fertile window may indicate ovulation has occurred as the rise in progesterone results in a change in the electrolytes of the cervical fluid.
We have heard from happy mamas who were able to successfully conceive using kegg despite their irregular cycles due to PCOS.

A kegg chart in which the mama with PCOS conceived. She was able to spot the “valley” in her daily readings to predict that she was in her fertile window.
While the diagnosis of PCOS can be devastating news, fortunately, there are many conventional and lifestyle approaches to symptom management and fertility. Women with PCOS successfully become mothers every day, thanks to the proper treatment and support. With kegg, women with PCOS who ovulate and have periods are able to use the trendline data to spot their fertile window-something that can be very challenging and frustrating with other fertility tracking methods. Even with curveballs like PCOS encountered on the fertility journey, know that you are not alone. At kegg, we are here to support you. Do you have a success story to share? We would love to hear from you. Email us at hello@kegg.tech